NIH Music-Based Intervention (MBI) Toolkit
This toolkit has been adapted from: Edwards E, St Hillaire-Clarke C, Frankowski DW, Finkelstein R, Cheever T, Chen WG, Onken L, Poremba A, Riddle R, Schloesser D, Burgdorf CE, Wells N, Fleming R, Collins FS. NIH Music-Based Intervention Toolkit: music-based interventions for brain disorders of aging. Neurology. 2023;13:10.
Introduction
In the past decade, the amount of research into the effects of the arts on health and well-being has increased.[1, 2] Nonpharmacologic approaches, such as music, continue to be explored for the treatment and symptom management of brain disorders of aging, including stroke,[3, 4] Parkinson’s disease (PD),[5–7] Alzheimer’s disease (AD), and Alzheimer’s disease-related dementias (ADRD).[8–10] There is evidence to support that music engages many different areas of the brain and may aid to strengthen brain networks and pathways involved in sensory and motor processes, emotion, affect, and memory.[11–14] Given that many of these domains can be affected by brain disorders of aging, music may therefore represent a cheaper, less invasive, and more accessible therapeutic avenue than traditional pharmacological approaches.
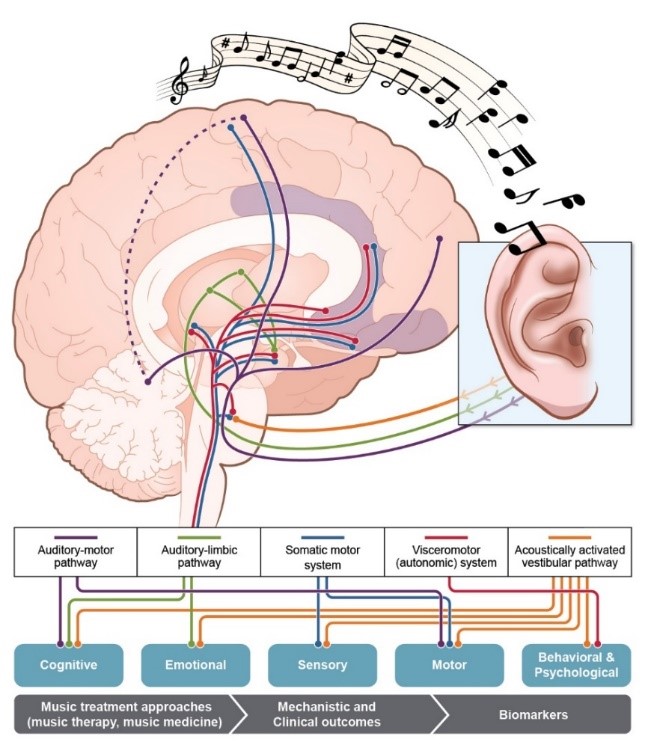
Figure 1. Pathways Underlying Neural and Physiological Responses to Music
(Adapted from: Koelsch S (2014) Nature Reviews Neuroscience 15 (3):170-180)
Aims of the NIH MBI Toolkit
To provide music and health researchers with a music-based intervention toolkit of recommendations in alignment with the NIH policy on rigor and reproducibility
To delineate the building blocks of music-based interventions
To define a core set of common data elements for music-based interventions protocols in various domains (e.g., cognition, emotion, motor function, sensory function)
To identify a core set of functional outcome measures and biomarkers focused on brain disorders of aging as a model system for music-based intervention research
To provide a framework and foundation for future music-based intervention research that can be applied across the lifespan and for various disease conditions
To create guidelines for intervention research on music and health
Significant strides have been made over the last decade to further the understanding, development, and effectiveness of music-based interventions (MBIs) for various disorders. For example, rhythmic auditory stimulation (RAS), a neurologic music therapy that involves the presentation of auditory rhythmic cues, has shown great promise for the treatment of gait disorders in individuals living with PD. RAS may reduce the number of freezing episodes and the number of falls in these patients.[7] Additionally, studies indicate that RAS may also provide some benefit to individuals with other neurological conditions where gait and postural stability are affected, such as stroke, traumatic brain injury, and AD. Moreover, singing can improve respiratory control and strengthening of muscles associated with swallowing and gait.[6, 7] Neurologic music therapy and melodic intonation therapy are used successfully for the rehabilitation of patients with nonfluent aphasia by stimulating their cognitive, emotional, and sensorimotor functions and by increasing their expressive language scores (e.g., repetition, sentence completion, naming nouns).[3, 15, 16] Other studies have explored whether MBIs could improve cognitive function in healthy aging and AD/ADRD[8, 9, 17, 18], as well as address the behavioral and psychological symptoms of AD (e.g., aggression, anxiety, irritability, and depression).[19]
Although MBIs have shown promise for symptom management in brain disorders of aging, large scale, rigorous, well-designed, and well-powered studies are needed to fully understand how music affects the brain and its therapeutic potential for these conditions. In the past five years, two Cochrane systematic reviews have concluded that MBIs have demonstrated benefits for people living with dementia and for people with acquired brain injury; however, these reviews have also highlighted the need for high-quality randomized trials before recommendations can be made for clinical practice.[20, 21] A more recent systematic review of MBIs for community-dwelling people living with dementia noted that inconsistency in study designs, procedures, and measures prevented specific conclusions to be drawn about potential therapeutic benefit.[22]
A major limitation to widespread application of MBIs has been the scarcity of data from rigorous, well-powered studies. Reports of the beneficial effects of MBIs have emerged either from anecdotal evidence or from small-scale clinical trials.[23] To further illustrate this point, the Agency for Healthcare Research and Quality (AHRQ) and the National Academies of Science, Engineering, and Medicine (NASEM) conducted a literature review in 2017 to assess the state of the science regarding nonpharmacologic approaches, including music, that might benefit the quality of life for people living with dementia. Their 2020 report, concluded from the 35 studies examined, that evidence was insufficient to draw conclusions about the benefits of music therapy for agitation, anxiety, depression, mood, and quality of life for people living with dementia.[24] Moreover, many of these studies had not been designed within a scientific and theoretical framework, and their results remain preliminary.
Another challenge for broad implementation of MBIs is the lack of consistent descriptive terminology. MBIs are divided into two major categories: music therapy and music medicine. Music therapy is an established health profession in which music is used within a therapeutic relationship to address physical, emotional, cognitive, and social needs of individuals, and includes the triad of music, clients, and qualified credentialed music therapists.[25] By contrast, music medicine is defined as having patients listen to prerecorded or live music, which is often managed by a medical professional other than a music therapist, such that the music plays the role of a medicine. Importantly, unlike music therapy, music medicine does not require a therapeutic relationship with the patient.[26–28] A clear distinction between these two types of MBIs is important for assessing treatment response and functional outcomes.[29]
Harnessing the therapeutic potential of music is of wide interest across the National Institutes of Health (NIH) (21 of NIH’s 27 Institutes and Centers have representatives to the Trans-NIH Music and Health Working Group (WG), part of the Sound Health Initiative).[30, 31] For MBIs to fulfill their potential, they must become more rigorous and replicable and align with the NIH Rigor and Reproducibility policy,[32] which will require the development of standards and tools that can be applied to interventional studies. The NIH, in partnership with the Renée Fleming Foundation and the Foundation for the NIH (FNIH), convened three workshops in 2021 to gather diverse and unbiased perspectives from five different communities representing content experts and a broad range of stakeholders (see Appendix for specific information on panel composition and discussion topics for each workshop). A direct outcome of these workshops is the development of the NIH MBI Toolkit: a set of guidelines and recommendations on what components need to be included in an MBI study to enhance data collection, allow for rigor, replicability, cross-study comparison and interpretation, and advance the biomedical research enterprise.[23, 33, 34] Other health research fields (e.g., physical therapy and traumatic brain injury) have benefited from such development of standards for interventional studies.[35, 36]